We were sitting around the supper table, playing True Colors. Laughter floated around as we voted on which person around the table would be most likely to arrive late, who has the most gadgets or who we would choose to be on a survival team.
Clank, clank, clank, clank. I got up to see who was at the gate. A man stood there in his rubber boots, an oversized shirt wrapped across his shoulders for extra warmth. His daughter had been in labor all day and they’d just arrived at clinic on a cot. I returned to the house to alert the others and together we headed down to clinic.
The pregnant lady was worn from laboring all day. Her family had stayed by her side and they too were worn. She encouraged her mom to sit and rest every moment she could. It was touching to see a patient caring for those around her.
Everything progressed well and within 2 hours, a little boy was born. His body was limp. I quickly clamped his cord and Abby and I took him over to the ER where Danny started giving rescue breaths. The baby had a heartbeat, but it wasn’t very fast, and he wasn’t taking any breaths yet. I checked on the mom, delivered her placenta, then returned to help Danny. Abby called James to come help, and before long James, Autumn and Daniel (Autumn’s dad who was visiting, also an EMT) arrived.

James and Daniel jumped right in and helped Danny. I went back to check on the mom. Autumn talked with the family and made sure a bed was ready for the mom in the hospital room. The new grandma walked her daughter over to her bed while I grabbed some more supplies for the rescue team in the ER. I cleaned up the delivery room and Abby started mopping.
The team in the ER was doing a fabulous job of giving rescue breaths, but the little guy just wasn’t breathing. Gradually his heartbeats had reached a normal rate. I helped stimulate him some, and at some points he’d move his foot a little, but mostly he was limp. Minutes ticked past. Occasionally he would gasp. We eagarly awaited the next breath a few minutes later.
We called a midwife to see if she had any tips for us to stimulate his breathing reflex. Her suggestions were things we’d already tried. He’d been born over an hour ago. James kept the family updated on the baby’s status and explained to them the gravity of his situation. They seemed to understand.
Next we called Dr Sutherland. He stayed on the phone with us for over an hour as the breaths became more and more regular. At last he breathed enough on his own that we could discontinue the rescue breaths.

Dr Sutherland prescribed a treatment for him, and we began to administrator some meds. I placed a feeding tube through the baby’s nose and gave him some milk. He was 2 hours old. Gradually the others left to return to our compound.
I took the baby to the hospital room and layed him on his mama’s chest. It was the first she’d held him since he was born. She smiled and cradeled him close. He contunued breathing, but I knew I’d need to continue monitoring him frequently throughout the night. I kept a monitor attached to his hand. It would sound an alarm whenever his heart rate or oxygen saturation would drop to low. I prayed the other patients in the hospital room would be able to sleep well, dispite my frequent trips in to check on the newborn.
I returned to the ER, picking up various items to tuck back in their proper places. I finished mopping the various rooms we’d been in, then sat down to chart. Danny returned with a pillow, blanket, waterbottle and phonecharger for me, and told me to call him if I needed anything throughout the night.
I finished charting, checked the baby and mama again, then layed down on the ER bed to try to grab several moments of sleep before it was time to feed the baby agian. I slept lightly, listening for the beeping monitor that alerted me each time he needed suctioned to help him breath easier, or my alarm each time he needed fed or given more medications. I noticed the baby breathed best when he was upright against his mom, his head on her chest.

Dawn arrived and with it came Mis Miranda. After giving her a report and turing the care over to her, I headed back to our compound for a shower and some breakfast. At 8:00 we gathered in Boss’s house to sing, read scripture and pray. Special prayers were lifted for the little boy, his family, and those of us caring for him.

James worked throughout the day trying to locate a hospital that had doctors and equipment available. We knew the baby needed more help than what we could give with our limited resources. Sometimes James found a willing doctor without equipment, other times he found a hospital that had equipment but no doctors. Other hospitals are simply closed due to gang control. Still, he kept checking.
Later that afternoon I was awoken from my nap with my cellphone ringing. Mis Ruth was on call, and told me she was having difficulty keeping the baby’s oxygen saturation up. I hurried down to clinic to help. We suctioned him and placed a nasal canula. Gradually his stats rose and we continued suctioning him so he could breath. He wasn’t responding as well, and he had a high fever for several hours now.
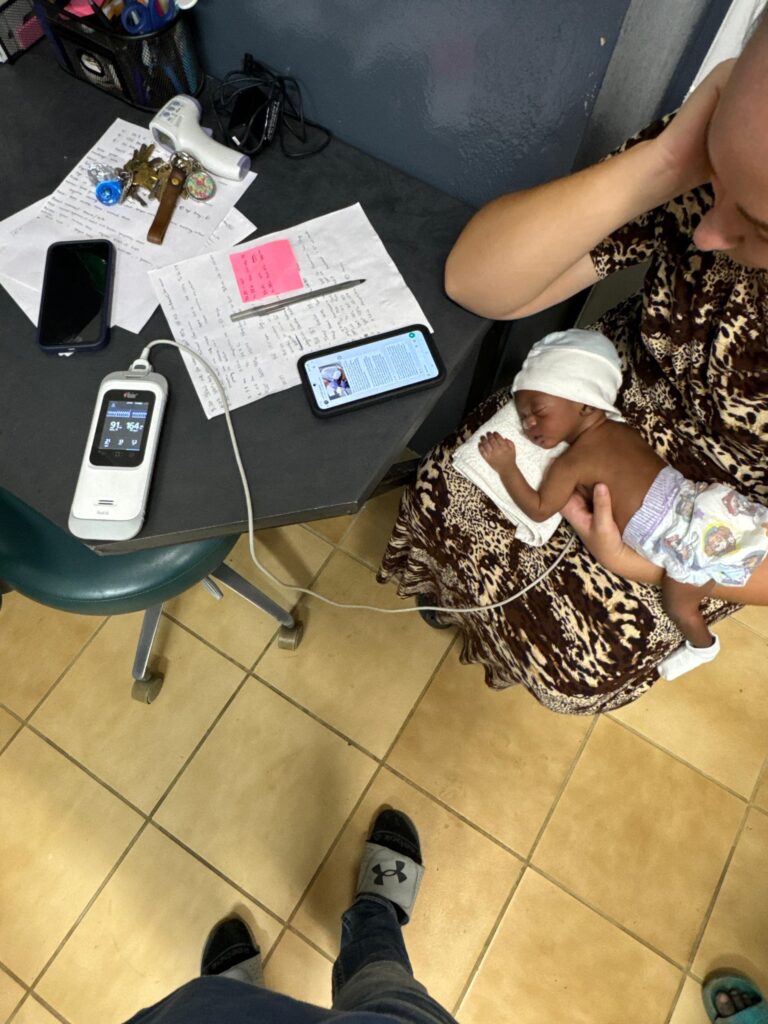
I held him in my lap, praying and wondering what his future would look like. Miranda and Stan stopped in to see how the baby was doing. We’d been messaging Dr Sutherland throughout the day and now we called him to give him a more thorough update. We discussed options of care since the search for a hospital to fly the baby to had come up empty.
I sat the baby up in my lap, and all of a sudden he stopped breathing. Something was blocking his airway. We started suctioning again, and gave some rescue breaths. James and Daniel walked in just then to check in on the baby, and they jumped right in to help.

Before to long, the baby started breathing on his own again. His stats rose and fell, and we gave oxygen as needed. The grandma came in every so often to check on him. He became more stable, and his fever was dropping. Dr Sutherland gave some more advice. We wrote some notes down, thanked him and ended our phone call.
I took the baby back into his mom and made sure she understood what had just happened. I showed the mom, aunt and grandma how to suction him if it got more difficult for him to breath, gave them insturctuons to call if they needed us for any reason, then we went home for supper.

After supper the grandpa knocked on the gate. Danny, Miranda and Stan went down to check the baby, suction him again and give him milk and meds. Danny stayed with him through the night, monitoring him and suctioning every so often to clear his airway. He also fed him and gave meds and oxygen as needed.
I awoke a little after 7 in the morning, feeling quite thankful for the opportunity for a full night of sleep. I noticed Miranda wasn’t in the house. I messaged her and she said she’d gone down at dawn and replaced Danny. She said the baby had had another rough night and was needing suctioned more frequently now, and it was harder to clear his airway. His fever was back and raging high. I quickly got ready and went down to help her.
The poor little guy looked so miserable. He was unresponsive agian and fluid was dripping from his nose. We suctioned and kept changing his position to help more fluid drain from his lungs. Stan showed up to help.
At 7:52 he stopped breathing. I called James, asking if he could come help as we started doing rescue breaths agian. We’d quickly pause from time to time to suction him change his position. Fluid poured from his lungs. Gradually his stats rose and he breathed again. His lungs still sounded junky.
Late the night before, James had found a hospital in Northern Haiti that had availability for the baby. The family had wanted to transfer him, but were torn with the logistics of other children to care for, work, and going to an unfamiliar area. This morning though, they were in agreement for continuing to pursue the option of transfer. James reached out to several contacts again.

We bathed the baby and cleaned up the ER. Staff and patients were arriving for the day. At 8:45 the others gathered for our morning singing and prayer time in the hallway as Miranda and I prepared to feed the baby. Halfway through the feeding, he seized and stopped breathing. Daniel and Stan rushed over to help. Stan handed me a stethoscope and I listened for a heartbeat. All I could hear was fluid in the lungs as the rescue breaths were given. Fluid continued to drain and we changed his position. Miranda and James checked for a heartbeat and couldn’t hear it. We stopped our interventions, stunned at what had just happened. Our hearts ached for the life that had lived only a few short hours, yet somehow there was serenity knowing he was free from struggle.
James went to talk to the mom while we wrapped the baby up and held him close. James came back and asked if Miranda or I could go talk with the mom. Her family had told her not to cry. I stepped over into the hospital room and saw the mom laying on her side, tears streaming down her face. Sitting down beside her on her bed I gave her a hug and layed my hand on her shoulder and told her it was ok to cry. My heart ached for her loss. I told her I was praying for her. I asked if she wanted to hold him, but she didn’t. She wanted to remember him alive. I sat with her for a bit longer, then returned to the ER.

I held his body a little longer, then lowered him into a cardboard box and closed the lid. I carried the box to the hospital room and layed it on the bed. The family was all gathered round. The grandpa thanked us repeatedly for our patience and care, and I assured them all we’d contunue to pray. I told them to ask if there was anything else we could do for them. Then I turned to care for the others who’d come to clinic that day
